UNDERSTANDING CANCER: What we know about colorectal cancer
ID
HNFE-643P (HNFE-1094P)
EXPERT REVIEWED
Did you know?
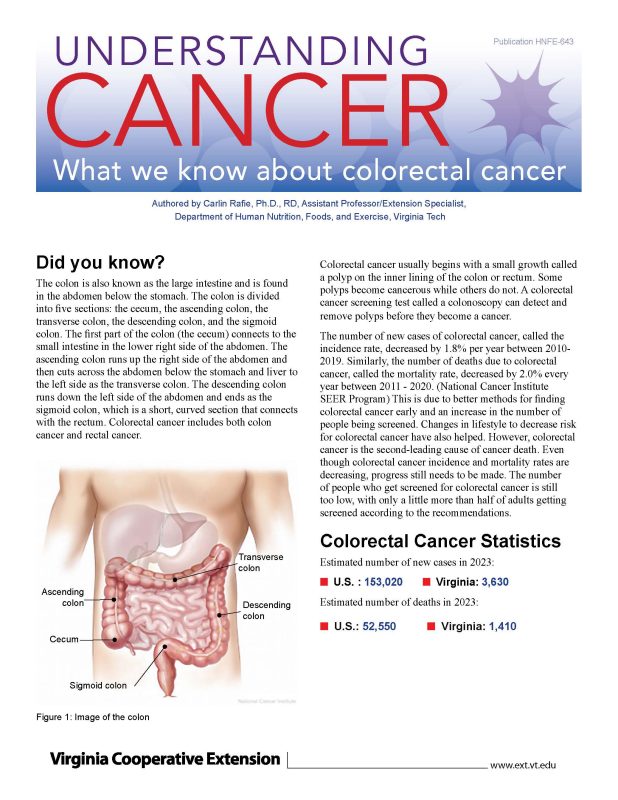
The colon is also known as the large intestine and is found in the abdomen below the stomach. The colon is divided into five sections: the cecum, the ascending colon, the transverse colon, the descending colon, and the sigmoid colon. The first part of the colon (the cecum) connects to the small intestine in the lower right side of the abdomen. The ascending colon runs up the right side of the abdomen and then cuts across the abdomen below the stomach and liver to the left side as the transverse colon. The descending colon runs down the left side of the abdomen and ends as the sigmoid colon, which is a short, curved section that connects with the rectum. Colorectal cancer includes both colon cancer and rectal cancer.

Colorectal cancer usually begins with a small growth called a polyp on the inner lining of the colon or rectum. Some polyps become cancerous while others do not. A colorectal cancer screening test called a colonoscopy can detect and remove polyps before they become a cancer.
The number of new cases of colorectal cancer, called the incidence rate, decreased by 1.8% per year between 2010-2019. Similarly, the number of deaths due to colorectal cancer, called the mortality rate, decreased by 2.0% every year between 2011 - 2020. (National Cancer Institute SEER Program) This is due to better methods for finding colorectal cancer early and an increase in the number of people being screened. Changes in lifestyle to decrease risk for colorectal cancer have also helped. However, colorectal cancer is the second-leading cause of cancer death. Even though colorectal cancer incidence and mortality rates are decreasing, progress still needs to be made. The number of people who get screened for colorectal cancer is still too low, with only a little more than half of adults getting screened according to the recommendations.
Colorectal Cancer Statistics
Estimated number of new cases in 2023:
■ U.S. : 153,020 ■ Virginia: 3,630
Estimated number of deaths in 2023:
■ U.S.: 52,550 ■ Virginia: 1,410
Five-year Survival Rate
(National Cancer Institute SEER Program)
The five-year survival rate tells what percent of people live at least five years after the cancer is found. The five-year survival rate for people in the U.S. diagnosed with colorectal cancer is 65 percent, or, in other words, 65 out of 100 people diagnosed with colorectal cancer will live at least 5 years.

The five-year survival rate increases to 90 percent when colorectal cancer is found before it has spread. In contrast, when the cancer is found after it has spread to distant organs, the five-year survival rate falls to only 15.6 percent.
Risk Factors for Colorectal Cancer (American Cancer Society 2018)
Several risk factors for colorectal cancer can be changed, while others cannot.
Risk factors that cannot be changed include:
✓ Age older than 50 years
✓ Inherited genetics that affect risk
✓ Family history of colorectal cancer
✓ Personal history of colorectal cancer or polyps in the colon, or inflammatory bowel disease.
✓ Eastern European Jewish or African American descent
Risk factors that can be changed include:
⊗ Being overweight or obese
⊗ Diet with a lot of processed meat and red meat and not enough vegetables and fruit
⊗ Physical inactivity
⊗ Tobacco use
⊗ Heavy alcohol use
Preventing Colorectal Cancer
(American Institute for Cancer Research, 2018)
https://www.aicr.org/resources/media-library/10-cancer-prevention-recommendations/
You can reduce your risk for colorectal cancer by getting screened and choosing a healthy lifestyle.
Get Screened
There are several ways to be screened for colorectal cancer. (See the section on screening recommendations.) A colonoscopy can detect and remove precancerous polyps, which significantly decreases the risk of developing cancer.
Know Your Risk
Talk with your physician to determine if you have increased risk of colorectal cancer.
Make Healthy Food Choices
Eat at least 2 1/2 cups of fruits and vegetables every day; doing so can decrease colon cancer risk by up to 25 percent. (van Duijnhoven 2009)
Choose lean meats (turkey, chicken, fish) more often than red meats (beef, pork, lamb).
Avoid processed meats, which include any meat preserved by smoking, curing, salting, or adding chemical preservatives. Examples include bacon, salami, sausages, hot dogs, and processed deli or luncheon meats.
When buying foods made from grains, such as bread, cereal, rice, or pasta, choose those made from whole grain. A whole grain has not been refined and contains all parts of the grain including the endosperm, germ, and bran.

Maintain a Healthy Body Weight
Reach and maintain a healthy weight for your height. A body mass index (BMI), measured by dividing your weight in kilograms by your height in meters squared, between 18.5 and 24.9 is generally considered a healthy weight. A BMI greater than 30 increases colorectal cancer risk by 41 percent. (Chan 2010) Use this link to calculate your BMI: http://mayoclinic.org/diseases-conditions/obesity/in-depth/bmi-calculator/itt-20084938.
Be Physically Active
Participate in at least 150 minutes of moderate-intensity aerobic exercise every week. Aerobic exercise makes you breathe faster and increases your heartbeat. Examples of aerobic exercise include brisk walking, jogging, swimming, and riding a bike. It is also important to do exercises that strengthen muscles two days per week and to avoid long periods of sitting or lying down during the day. (American College of Sports Medicine 2018)
Don’t Smoke
Both current and former smokers have over twice the risk of developing colorectal cancer compared with people who never smoked. (Botteri 2008) If you smoke, ask your physician for guidance on how to quit. Check out this site from the American Lung Association for resources on quitting smoking: http://www.lung.org/stop-smoking/i-want-to-quit/.
Avoid Heavy Alcohol Use
Research shows that individuals who drink more than one standard alcoholic drink a day (e.g., a 5-ounce glass of wine; a 12-ounce regular beer; or 1.5 ounces of 80 proof spirits) have a 41 percent greater risk of developing colorectal cancer compared with nondrinkers. If you drink, limit the amount you drink in a single sitting. The American Institute of Cancer Research analysis of 19 research studies showed a significant increase in risk for colorectal cancer with alcohol intake of 30 grams (e.g. two 5-ounce glasses of wine; two 12-ounce regular beers; or 3.0 ounces of 80 proof spirits) or more a day. (AICR 2018)
Types of Colorectal Cancer
(American Cancer Society 2018)
https://www.cancer.org/cancer/colon-rectal-cancer/about/what-is-colorectal-cancer.html
There is one primary type of colorectal cancer.
- Adenocarcinoma. This type of colorectal cancer develops in the mucus-producing cells of the colon or rectum. This is by far the most common type; 9.5 out of 10 colorectal cancers are adenocarcinomas.
Several other less common types of cancer may start in the colon or rectum, including:
- Carcinoid tumors, which start in neuroendocrine cells found in the colon or rectum.
- Gastrointestinal stromal tumors, which start in special cells in the wall of the gastrointestinal tract called “interstitial cells of Cajal.”
- Lymphomas, which start in cells in of the immune system that reside in the colon or rectum.
- Sarcomas, which start in blood vessels, muscle layers, or other connective tissues in the wall of the colon and rectum.
Symptoms of Colorectal Cancer
(American Cancer Society 2018)
Symptoms may not be present until colorectal cancer has already progressed. Regular screening helps prevent or detect colorectal cancer at an early stage.
| Common Symptoms of Colorectal Cancer |
|---|
A change in bowel habits lasting more than a few days Rectal bleeding Rectal bleeding Blood in the stool Cramping Urge for a bowel movement but lack of relief in doing so Weakness Fatigue Unintended weight loss |
Early Detection and Screening
(American Cancer Society 2018)
There are very good ways of detecting colorectal cancer before there are any signs or symptoms. This is called screening. These include stool-based tests (including the fecal occult blood test, the fecal immunochemical test, and stool DNA tests), and visual tests (such as flexible sigmoidoscopy, colonoscopy, and CT colonography). See the Glossary of Terms for a description of these tests. In the case of colonoscopy, early stage cancers and small growths in the colon called polyps that may become cancer can be removed. Screening should begin at age 45 for people of average risk, and all people should be screened for colorectal 4 cancer according to the screening guidelines (see figure 4). Those who have additional risk factors should speak with their doctor about starting screening earlier.
Early Detection & Screening U.S Preventive Services Task Force Guidelines for adults age 45-75 years of age and older who are at average risk:* Stool-based test (FOBT, FIT, sDNA-FIT) every year OR CT Colonography or Flexible Sigmoidoscopy every 5 years OR Colonoscopy every 10 years

Diagnosis
(American Cancer Society 2018)
https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/how-diagnosed.html
If the results of a colorectal cancer screening test shows something abnormal, a doctor will recommend further tests. A diagnostic colonoscopy may be conducted when something abnormal has been found. During this exam, which is similar to a screening colonoscopy, suspicious-looking areas in the colon or rectum can be removed (biopsied) and examined to make a diagnosis. If a biopsy shows that cancer is present, further tests will be done to see if and how far the cancer has spread and to stage the cancer. The stage of the cancer describes how much cancer there is and if it has spread. The earliest stage of colorectal cancer is stage 0, followed by stages I (1) through IV (4). The higher the number, the more cancer there is and the more it has spread.
Treatment
(National Cancer Institute 2018)
https://www.cancer.gov/types/colorectal/patient/colon-treatment-pdq#section/_135
Treatment of colorectal cancer depends on the type and stage of cancer. Treatments can be local, meaning they do not affect other parts of the body, or systemic, meaning they spread throughout the body.
Local Therapies
Surgery
Surgery is often used for earlier stage colorectal cancers. Polyps and early stage cancers can be removed with a polypectomy or local excision during a colonoscopy. More advanced cancers may require removal of part or all of the colon or rectum, along with nearby lymph nodes. This is called a colectomy.
Radiation
Radiation uses high-energy particles to destroy cancer cells. Radiation may be from external-beam radiation that consists of a certain number of treatments given over a set period of time, or internal radiation that uses radioactive implants placed in or near the cancer tissue. Radiation therapy is more often used to treat rectal cancer than colon cancer.
Systemic Therapies
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. Drugs used to treat colorectal cancer are given through injection into the blood (intravenous). A chemotherapy regimen may use one or a combination of drugs and consists of a specific number of cycles given over a period of time. It may be given after surgery (adjuvant chemo) or before surgery (neoadjuvant chemo).
Targeted therapy drugs
Newer cancer-fighting drugs have been developed that target specific gene and protein changes in the cells that cause colorectal cancer. These may be given as intravenous injections or taken as a pill.
Immunotherapy
These drugs help a person’s own immune system recognize and destroy cancer cells. They may be used to treat people with more advanced cancer and those who have not responded to other treatment.
Treatment for colorectal cancer may involve one or a combination of these treatment options.
Glossary of Terms
Biopsy – removal of a sample of cells or tissue for examination to determine the presence or extent of disease.
Carcinoid tumor – a tumor that starts in neuroendocrine cells, which are cells that are like both nerve cells and hormone-making cells. The digestive system has more neuroendocrine cells than any other part of the body and is where carcinoid tumors most often start. For more information see: https://www.cancer.org/cancer/gastrointestinal-carcinoid-tumor/about/what-is-gastrointestinal-carcinoid.html.
Colonoscopy – a test conducted by a doctor that looks at the entire colon and rectum using a flexible tube with a light and small video camera, which are put into the colon through the anus.
CT colonography – a screening test for colorectal cancer that uses computed tomography (CT) to take multiple pictures (x-rays) that are then combined by a computer to create detailed two- and three-dimensional images of the inside of the colon and rectum. Suspicious findings must be followed up with a colonoscopy.
Gastrointestinal stromal tumor (GIST) – a tumor that starts in special cells in the wall of the gastrointestinal tract called the interstitial cells of Cajal. For more information see: https://www.cancer.org/cancer/gastrointestinal-stromal-tumor/about/what-is-gist.html
Fecal occult blood test (FOBT) – a test that checks for blood in the stool using a chemical reaction. Certain drug and dietary restrictions are required for this test, and stool sample collection can be done at home. A positive test may be an indication of colorectal cancer and must be followed up with a colonoscopy.
Fecal immunochemical test (FIT) – a test that checks for blood in the stool using an immune reaction to the hemoglobin protein found in red blood cells. No drug or dietary restrictions are required for this test, and stool sample collection can be done at home. A positive test may be an indication of colorectal cancer and must be followed up with a colonoscopy.
Flexible sigmoidoscopy – a test conducted by a doctor that looks at the lower portion of the colon and rectum using a flexible tube with a light and small video camera that are put into the colon through the anus. If precancerous polyps or colorectal cancer is found, a colonoscopy is required to look at the remainder of the colon.
Stool DNA test – a colorectal cancer screening test that looks for DNA from cancer or polyp cells. A suspicious finding must be followed up with a colonoscopy.
Information Resources
American Cancer Society http://www.cancer.org/cancer/colon-rectal-cancer/about.html
American Institute for Cancer Research http://www.aicr.org
Centers for Disease Control and Prevention http://www.cdc.gov/cancer/colorectal
National Colorectal Cancer Roundtable http://nccrt.org/
Surveillance, Epidemiology, and End Results Program http://www.seer.cancer.gov
U.S. Preventive Services Task Force http://www.uspreventiveservicestaskforce.org/Page/Document/Recommendation
StatementFinal/ colorectal-cancer-screening
References
American Cancer Society. 2018. “Can Colorectal Polyps and Cancer Be Found Early?” Last revised June 29, 2020. https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/detection.html.
American Cancer Society. 2018. “Cancer Statistics Center: Colorectum.” https://cancerstatisticscenter.cancer.org/?_ga=1.122799371.1049472307.1455672429#!/cancer-site/Colorectum.
American Cancer Society. 2018. “Colorectal Cancer Risk Factors.” Last revised July 19, 2023. https://www.cancer.org/cancer/types/colon-rectal-cancer/causes-risks-prevention/risk-factors.html.
American Cancer Society. 2018. “Colorectal Cancer Signs and Symptoms.” Last revised June 29, 2020. https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/signs-and-symptoms.html.
American Cancer Society. 2018. “Key Statistics for Colorectal Cancer.” Last revised January 13, 2023. https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html.
American Cancer Society. 2018. “What is colorectal cancer?” Last revised June 29, 2020. https://www.cancer.org/cancer/types/colon-rectal-cancer/about/what-is-colorectal-cancer.html.
American College of Sports Medicine. 2018. “Updated Physical Activity Guidelines Now Available.” News release. https://www.acsm.org/news-detail/2018/11/12/updated-physical-activity-guidelines-now-available.
American Institute for Cancer Research. 2018. “Cancer Prevention Recommendations.” http://www.aicr.org/can-prevent/what-you-can-do/10-recommendations.html?_ga=2.32839102.129
Botteri, Edoardo, Simona Iodice, Sara Raimondi, Patrick Maisonneuve, and Albert B. Lowenfels. 2008. “Cigarette Smoking and Adenomatous Polyps: A Meta-analysis.” Gastroenterology 134(2), 388–395. https://doi.org/10.1053/j.gastro.2007.11.007.
Chan, Andrew T., and Edward L. Giovannucci. 2010. “Primary Prevention of Colorectal Cancer.” Gastroenterology, 138(6), 2029–2043.e10. https://doi.org/10.1053/j.gastro.2010.01.057.
National Cancer Institute. 2018. “Colon Cancer Treatment.” Last revised May 4, 2018. https://www.cancer.gov/types/colorectal/patient/colon-treatment-pdq-section/_135.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. n.d. “Cancer Stat Facts: Colorectal Cancer.” Accessed on July 13, 2018. https://seer.cancer.gov/statfacts/html/colorect.html.
U.S. Cancer Statistics Working Group. 2015. “United States Cancer Statistics: 1999–2012 Incidence and Mortality Web-based Report.” https://www.cdc.gov/uscs.
van Duijnhoven, Franzel J. B., H. Bas Bueno-de-Mesquita, Pietro Ferrari, Mazda Jenab, Hendriek C. Boshuizen, Martine M. Ros, Corinne Casagrande et al. 2009. “Fruit, Vegetables, and Colorectal Cancer Risk: The European Prospective Investigation into Cancer and Nutrition.” American Journal of Clinical Nutrition, 89(1), 1441–1452. https://doi.org/10.3945/ajcn.2008.27120.
Virginia Cooperative Extension materials are available for public use, reprint, or citation without further permission, provided the use includes credit to the author and to Virginia Cooperative Extension, Virginia Tech, and Virginia State University.
Virginia Cooperative Extension is a partnership of Virginia Tech, Virginia State University, the U.S. Department of Agriculture (USDA), and local governments, and is an equal opportunity employer. For the full non-discrimination statement, please visit ext.vt.edu/accessibility.
Publication Date
February 27, 2024